Managing Diabetes in Athletes: A Review of the AMSSM Position Statement

Caring for athletes with diabetes requires a collaborative, multi-disciplinary approach, involving primary care physicians, endocrinologists, diabetes educators, and more. However, primary care sports medicine physicians are uniquely positioned to lead the way in managing this complex care, thanks to their specialized training that bridges both diabetes management and sports medicine. In 2022, the American Medical Society for Sports Medicine (AMSSM) released a position statement on the care of athletes with diabetes, offering invaluable guidance for healthcare providers. In this post, we’ll review key takeaways from this position statement and explore how it can serve as a foundational resource for professionals managing this unique patient population.
Highlights from AMSSM’s Position Statement on the Care of Athletes/Athletic Person with Diabetes
The following are the key points that the authors highlight in the care of the diabetic athlete:
The number of athletes with type 1 diabetes participating in high school and college sports is not well known, but seems to be the same as the percentage of individuals with type 1 diabetes in the general population.
- Dabelea et. al. note that the prevalence of type 1 diabetes in individuals 19 years and younger is 3.22 (95% CI, 3.11-3.34) per 10001
- Dr. Thomas Trojian conducted a pilot study in 2018 which showed that the prevalence of type 1 diabetes among college-age athletes is 3.42 (±2.36 SD) per 10002
Medical evaluation is not needed before low to moderate exercise in patients with diabetes who receive regular care.
- Historically, the rationale for pre-exercise screening in patients with diabetes was to limit/prevent the risks of an acute cardiovascular event and hypo/hyperglycemia.
- Recent evidence suggests that the risk of adverse events is low, and for the majority of individuals with diabetes, the benefits of exercise outweigh the associated risks3,4,5.
- Screening for cardiovascular disease (CVD) in asymptomatic individuals engaging in low-to-moderate intensity exercise has not demonstrated a reduction in the incidence of cardiac events.
- Indications for Pre-Exercise Screening per AMSSM Position Statement:
- Patients with symptoms of CVD, regardless of exercise intensity level.
- Individuals attempting to begin a vigorous exercise program.
- Individuals who are increasing from a relatively sedentary level of activity to a more vigorous level of exercise.
Resistance exercise for patients with type 1 diabetes lowers A1c levels.
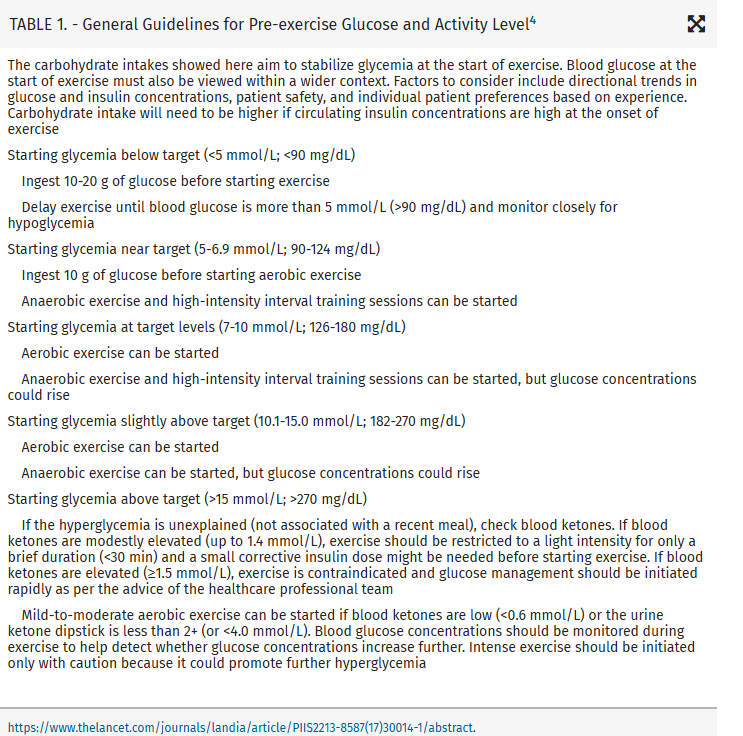
- Aerobic exercise typically leads to a rapid reduction in glucose levels usually within 45 minutes of starting exercise.
- Anaerobic exercise leads to an increase in lean muscle mass and strength which translates to enhanced glucose uptake/restoration of glycogen stores, improved athletic performance, heightened insulins sensitivity, and improvement in A1c after 6 months6.
- It is important to note that despite the above long term benefits of anaerobic exercise, short term it can result in hyperglycemia because of catecholamine release leading to rapid mobilization of liver and muscle glycogen.
- Therefore, it is important to counsel your athletes about the different effects of exercise on glucose levels as well as necessary insulin adjustments.
- In 2018, Ostman et al performed a meta-analysis that included 323 individuals with type 1 diabetes who participated in either aerobic, resistance training, or HITT exercises and found that for best long term glycemic management and cardiorespiratory fitness gains, a combination of all 3 types of exercise showed more significant benefit than any one type of exercise alone.
- Unsurprisingly, the subgroup analysis showed a more significant improvement in participant’s A1c if their starting A1c was > 8.5%.
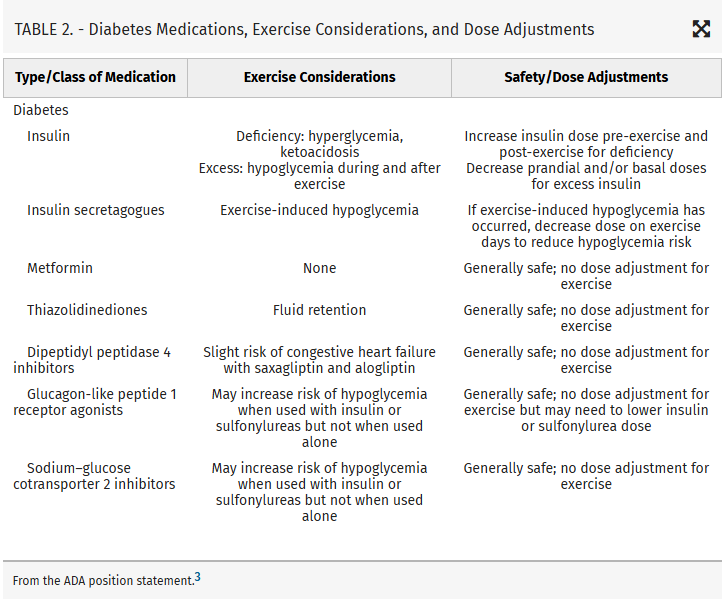
Reduction in basal insulin is needed with vigorous exercise
Newer medications for type 2 diabetes generally do not need an adjustment with exercise.
Every school should have an emergency action plan (EAP) for athletes with diabetes and possible hypoglycemia.

- Click here for a Sample EAP.
To see the full position statement click on the link below:
AMSSM Position Statement on the Care of the Athlete with Diabetes
~ Harness the power of your journey, and never stop pushing boundaries. ~
Dr. Richard Edgar
***Disclaimer: Always consult with your healthcare provider before making any changes to your treatment or management plan.
References:
- Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311:1778-1786.
- Trojan TH. Prevalence of type 1 DM in student-athletes: AMSSM oral research poster presentation. Clin J Sports Med. 2018;28:210.
- Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: A position statement of the American Diabetes Association. Diabetes Care. 2016;39:2065-2079.
- Muhlestein JB, Lappe DL, Lima JA, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA. 2014;312:2234-2243.
- Young LH, Wackers FJ, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA. 2009;301:1547-1555.
- Sigal RJ, Kenny GP, Boule NG, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med. 2007; 147:357-369.
