How My Menstrual Cycle Affects Insulin's Action -Special Considerations for the Female Athlete with Diabetes

How My Menstrual Cycle Affects Insulin's Action
Have you ever wondered if your menstrual cycle has an affect on your diabetes? Do you notice that during certain times of the month that your blood sugar levels seem to always run higher no matter what actions you take? You are not making it up! It is well documented in the medical literature that some women complain of variations in the blood glucose levels which correspond to the various phases of their menstrual cycle 1-6. In this blog post we explore how the various hormones during a woman's menstrual cycle affect insulin action and discuss actions one can take to help maintain more normal glucose levels.
Understanding the menstrual cycle and hormonal affects on insulin
To understand how your menstrual cycle affects diabetes management we must first understand the hormones involved in the menstrual cycle. For simplicity, the menstrual cycle can be broken down into 2 phases: the follicular phase and the luteal phase. The hormone levels, particular estrogen and progesterone, in these phases vary allowing for ovulation and preparing the uterine lining for implantation of a fertilized egg. These hormone variations can have a drastic effect on your glucose levels and subsequently your diabetes control. Lets take a closer look at each phase of the menstrual cycle below.
- Follicular Phase (Days 1-14)
- This stage spans from the first day of your menses (period) to midcycle ovulation (egg release).
- During menses, estrogen and progesterone levels are low. Follicle-stimulating hormone (FSH) levels begin to rise stimulating follicle development in the ovaries.
- Approximately day 5 or 6 (mid-follicular phase), levels of estrogen begin to increase as follicles mature in the ovaries.
- Estrogen causes the uterine lining to thicken in preparation for a potential pregnancy.
- Around day 12, luteinizing hormone and estrogen surge triggering ovulation.
- Luteal Phase (Days 15-28)
- The luteal phase spans from the time of ovulation to the start of your next menses.
- Estrogen levels drop slightly after ovulation.
- The rupture follicle (corpus luteum) begins to produce progesterone and estrogen.
- Progesterone continues to thicken the uterine lining.
- If fertilization occurs, the fertilized egg implants into the uterus and continues to produce hormones.
- If fertilization does not occur, the corpus luteum degrades --> hormone levels drop --> menses occurs.
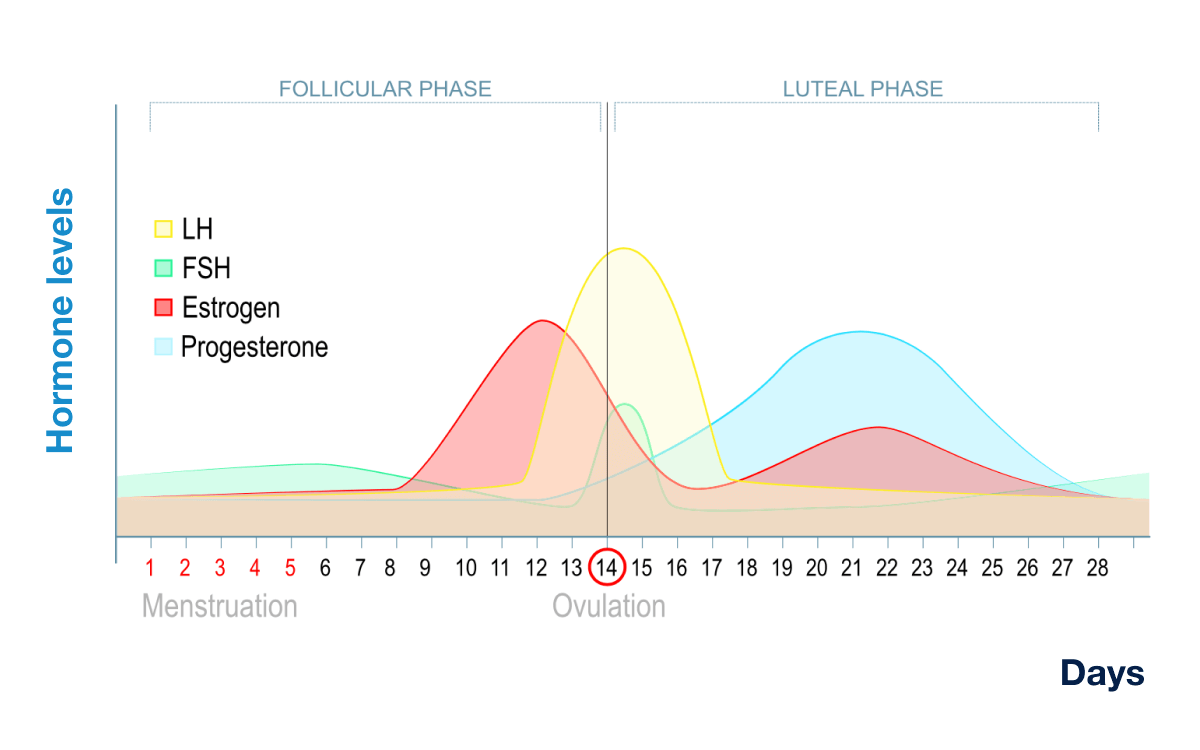
The pathophysiology of glucose changes during the menstrual cycle for woman living with type 1 diabetes continues to not be well understood; however, is strongly linked to changes in insulin sensitivity. Progesterone rises during the luteal phase and is considered to be the cause of increased insulin resistance leading to higher blood sugar levels. Conversely, when progesterone levels fall in the early follicular phase, higher insulin sensitivity is noted leading to lower blood sugar levels 4-5.
Similarly, fluctuations in estrogen levels during the menstrual cycle are thought to play a role in glucose variations and insulin sensitivity. An increase in estradiol between the follicular and luteal phases is associated with higher glucose levels. In a prospective study of 259 premenopausal woman, estradiol levels were positively associated with insulin resistance peaking during the luteal phase7.
Insulin Management Changes during menstrual cycle
It is proposed that more than one-half of premenopausal women with type 1 diabetes require specific alterations to their insulin management during their menstrual cycle to avoid recurrent hyper- and hypoglycemia. A recent 2022 observational study evaluated glucose variability during the menstrual cycle using a continuous glucose monitor (CGM) to further understand glucose variability during the menstrual cycle. They observed 26 woman with type 1 diabetes during 62 menstrual cycles. They found that the time spent in range decreased from the beginning to the end of the menstrual cycle. Hyperglycemia was most notable at the end of the menstrual cycle, during the luteal phase. Furthermore, the risk of hypogylcemia was greatest during the mid-follicular phase8.
I think the reason this is not addressed more directly is multifactorial; however, I hope that we can give you some basic information to feel more empowered to speak with your care team on this topic. With our basic understanding of how hormones affect glucose levels we will discuss some general insulin management changes you can discuss with your endocrinologist to optimized your own diabetes management. If you have a CGM, looking back at your trends during your menstrual cycle can be helpful to evaluate your particular response and when to best implement these changes. As always, we recommend you consult with your provider prior to making these changes.
--> Multiple Daily Injections
Increased insulin resistance means that you need more insulin to have the same effect. For those individuals treating their diabetes with multiple daily insulin injections the question becomes which insulin(s) do you need to alter to achieve optimal glucose management. I am assuming that you are on a basal/bolus regimen which will include a long acting insulin (i.e. Lantus, Basaglar, Levemir, etc) and a shorter acting insulin (Humalog, Novolog, Apidra, etc). I would argue that changes to your long acting insulin will have the biggest bang for your buck with lower risk for hypoglycemia. Increasing your basal insulin by 25-50% during the luteal phase may help offset the hormonal effects of increased insulin resistance.
--> Insulin Pump Users
Insulin pumps only use short acting insulins and therefore you do not need to decide which insulin needs to be changed; however, they follow a similar basal and bolus pattern. If you are not aware of this yet, you can set different programs in your insulin pump (refer to your individual pump manual) that have built in basal/bolus settings for various scenarios. Again, increasing your basal insulin by 25-50% during the luteal phase is recommended; however, instead of manually changing this every month you can simply have a separate basal/bolus program that you switch to during the luteal phase and then switch back to your "normal" program at the start of your menses. Click on the YouTube video below to see an example of how you can set up personal profiles using the t:slim X2 insulin pump. I use tandem as an example because it is the insulin pump I use; however, each insulin pump will have similar capabilities. Refer to your insulin pump's instruction manual for more information.
With the advent of closed loop monitoring, insulin pumps are now able to detect changes in your glucose in real time and either bolus for acute episodes of hyperglycemia as well as make small alterations to basal insulin rates to combat higher than normal glucose levels. While this has been an incredible advancement in the technology available to individuals with diabetes, I would argue that being proactive rather than reactive is best.
Concluding Remarks
Understanding the connection between your menstrual cycle and blood glucose fluctuations is a vital step in optimizing your diabetes management. While each woman’s experience may vary, recognizing patterns and anticipating changes—particularly during the luteal phase—can help reduce frustration and improve outcomes. Whether you use multiple daily injections or an insulin pump, adjusting your insulin regimen in response to hormonal shifts may make a significant difference helping optimize athletic performance. Most importantly, don’t hesitate to address this topic with your care team. With the right tools, knowledge, and support, you can take control of your cycle-related glucose changes and feel more confident in your diabetes journey.
~ Harness the power of your journey, and never stop pushing boundaries. ~
Dr. Richard Edgar
***Disclaimer: Always consult with your healthcare provider before making any changes to your treatment or management plan.
References:
- Lunt H, Brown LJ. Self-reported changes in capillary glucose and insulin requirements during the menstrual cycle. Diabet. Med. J. Br. Diabet. Assoc 1996; 12(6): 525-530.
- Herranz L, Saiz-de-Ibarra L, Hillman N, Gaspar R, Pallardo LF. Glycemic changes during menstrual cycles in women with type 1 diabetes. Med. Clin. (Barc.) 2016;146(7):287-291.
- Widom B, Diamond MP, Simonson DC. Alterations in glucose metabolism during menstrual cycle in women with IDDM. Diabetes Care. 1992;15(2):213-220.
- Goldner WS, Kraus VL, Sivitz WI, Hunter SK, Dillon JS. Cyclic changes in glycemia assessed by continuous glucose monitoring system during multiple complete menstrual cycles in women with type 1 diabetes. Diabetes Technol Ther. 2004;6(4):473-480.
- Barata DS, Adan LF, Netto EM, Ramalho AC. The effect of the menstrual cycle on glucose control in women with type 1 diabetes evaluated using a continuous glucose monitoring system. Diabetes Care. 2013:36(5):e70.
- Brown SA, Jiang B, McElwee-Malloy M, Wakeman C, Breton MD. Fluctuations of hypergylcemia and insulin sensitivity are linked to menstrual cycle phases in women with T1D. J Diabetes Sci Technol. 2015:9(6):1192-1199.
- Yeung EH, Zhang C, Mumford SL, et al. Longitudinal study of insulin resistance and sex hormones over the menstrual cycle. the BioCycle Study. J Clin Endocrinol Metab. 2010;95(12):5435-5442.
- Tatulashvili S, Baptiste Julla J, Sritharan N, Rezgani I, Levy V, Bihan H, Riveline JP, Cosson E. Ambulatory Glucose Profile According to Different Phases of the Menstrual Cycle in Women Living With Type 1 Diabetes. J Clin Endocrinol Metab. 2022 Sep 28;107(10):2793-2800. doi: 10.1210/clinem/dgac443. PMID: 35869507.
